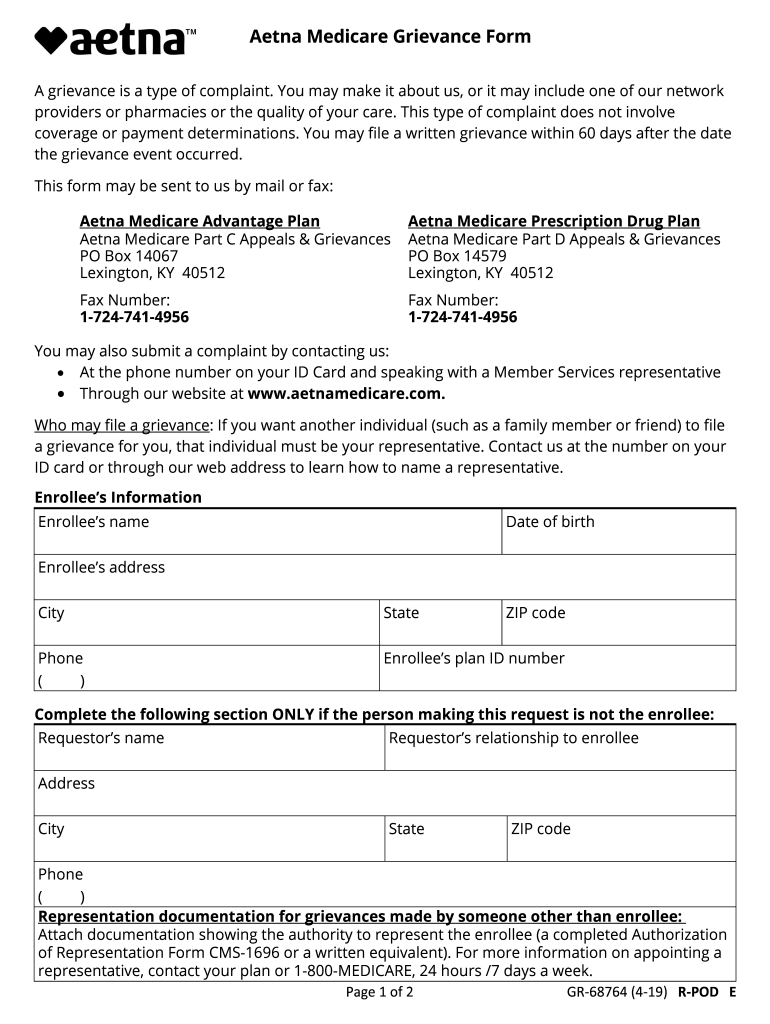
Aetna Medicare Reconsideration Form
Aetna Medicare Reconsideration Form - You must submit appeals within 60 days of the date of denial notice. Providers in the aetna network have the right to appeal denied medical item or service authorizations or medicare part b prescription drug for members. Your doctor may ask us for an appeal on your behalf. Coordination of benefits (cob) employee assistance program (eap) medicaid disputes and appeals. Web find forms and applications for health care professionals and patients, all in one place. You may mail your request to: Web helping patients to appeal denials on medicare authorization or precertification requests. Web lexington, ky 40512 payment appeals for contracted provider requests if you have a dispute around the rate used for payment you have received, please visit health care professional dispute and appeal process. You have 60 calendar days from the date of. Make sure to include any information that will support your appeal.
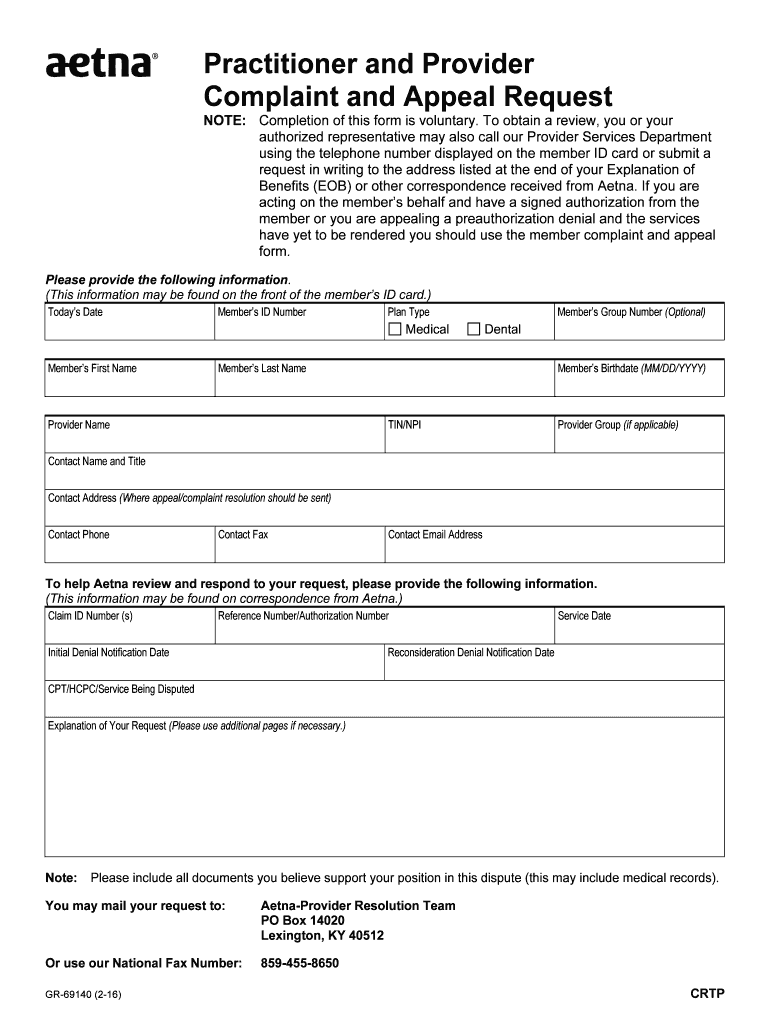
Who may make a request: Practitioner and provider compliant and appeal request Web complaints and coverage requests please come to us if you have a concern about your coverage or care. Web helping patients to appeal denials on medicare authorization or precertification requests. See how to get started 1 if you don't have creditable coverage for 63 days or more, you may have to pay a late enrollment penalty. Providers in the aetna network have the right to appeal denied medical item or service authorizations or medicare part b prescription drug for members. Web to obtain a review, you’ll need to submit this form. Because aetna medicare (or one of our delegates) denied your request for coverage of a medical item or service or a medicare part b prescription drug, you have the right to ask us for an appeal of our decision. You have 60 calendar days from the date of. Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial.
This may be medical records, office notes, discharge. Providers in the aetna network have the right to appeal denied medical item or service authorizations or medicare part b prescription drug for members. Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial. Web lexington, ky 40512 payment appeals for contracted provider requests if you have a dispute around the rate used for payment you have received, please visit health care professional dispute and appeal process. Web complaints and coverage requests please come to us if you have a concern about your coverage or care. You must submit appeals within 60 days of the date of denial notice. Web to obtain a review, you’ll need to submit this form. Coordination of benefits (cob) employee assistance program (eap) medicaid disputes and appeals. Who may make a request: Because aetna medicare (or one of our delegates) denied your request for coverage of a medical item or service or a medicare part b prescription drug, you have the right to ask us for an appeal of our decision.
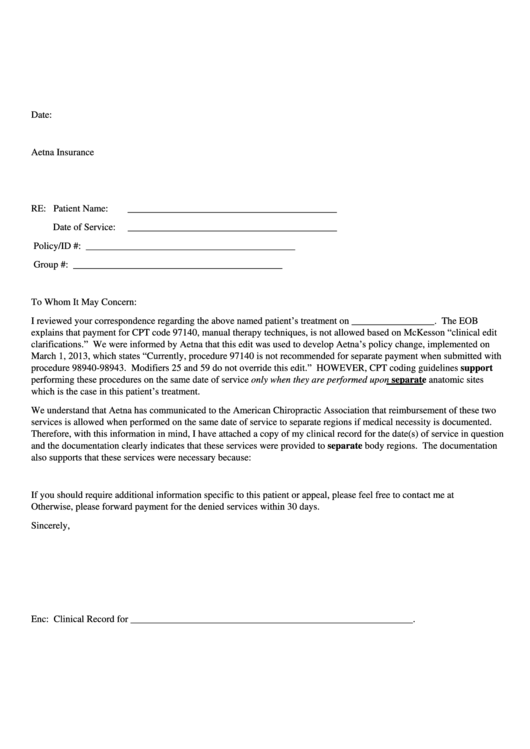
Appeal Letter Sample For Reconsideration HQ Printable Documents
Hospital discharge appeals all medicare patients can appeal an inpatient hospital discharge decision. Or use our national fax number: Make sure to include any information that will support your appeal. Call us at the number on your member id card, or learn more first. This may be medical records, office notes, discharge.
Aetna GR690251 CO 2016 Fill and Sign Printable Template Online US
This may be medical records, office notes, discharge. Web complaints and coverage requests please come to us if you have a concern about your coverage or care. Because aetna medicare (or one of our delegates) denied your request for coverage of a medical item or service or a medicare part b prescription drug, you have the right to ask us.
Aetna Appeal Letter Sample Templates
Practitioner and provider compliant and appeal request Make sure to include any information that will support your appeal. Or use our national fax number: Web complaints and coverage requests please come to us if you have a concern about your coverage or care. You must submit appeals within 60 days of the date of denial notice.
Medicare Enrolment Form 3101 Form Resume Examples GX3GDwy8xb
Providers in the aetna network have the right to appeal denied medical item or service authorizations or medicare part b prescription drug for members. Call us at the number on your member id card, or learn more first. Because aetna medicare (or one of our delegates) denied your request for coverage of a medical item or service or a medicare.
Aetna Medicare Pa Forms Universal Network
You have 60 calendar days from the date of. Your doctor may ask us for an appeal on your behalf. Who may make a request: Web complaints and coverage requests please come to us if you have a concern about your coverage or care. Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial.
Fillable Aetna Denied Appeal Letter Template printable pdf download
See how to get started 1 if you don't have creditable coverage for 63 days or more, you may have to pay a late enrollment penalty. Web find forms and applications for health care professionals and patients, all in one place. Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial. Because aetna medicare (or.
Aetna Medicare Complaint Team Fill Out and Sign Printable PDF
Address, phone number and practice changes. If your complaint involves a broker or agent, be sure to include the name of the person when filing your grievance. Web helping patients to appeal denials on medicare authorization or precertification requests. See how to get started 1 if you don't have creditable coverage for 63 days or more, you may have to.
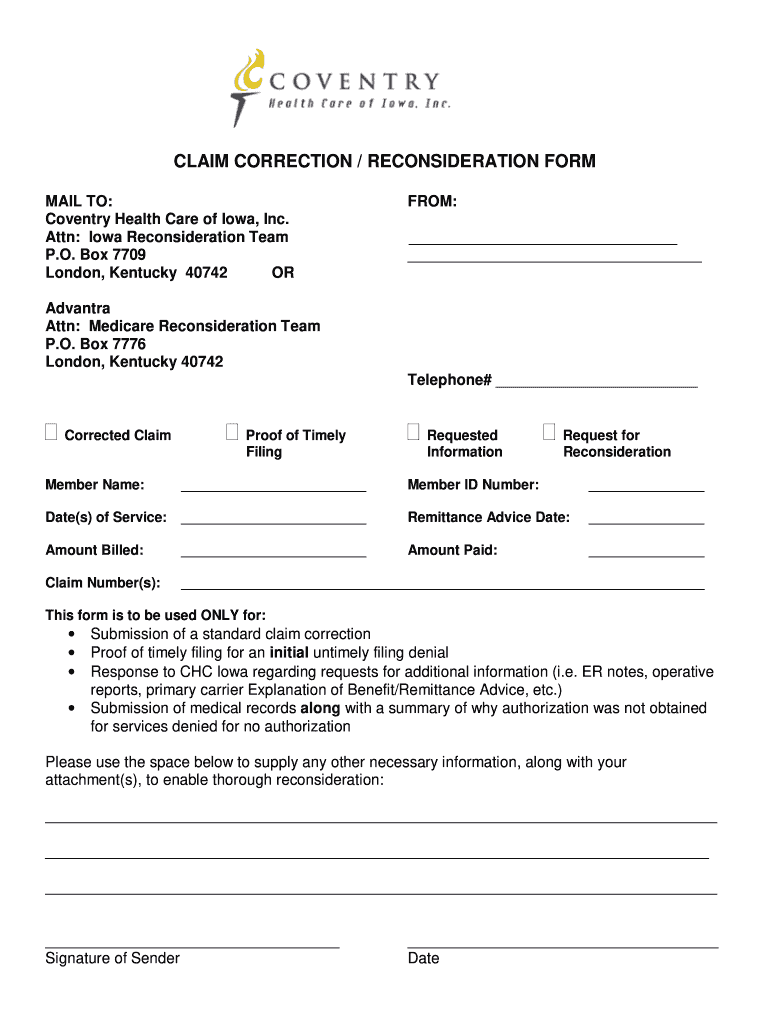
Aetna Reconsideration Form Fill Online, Printable, Fillable, Blank
Web reconsideration denial notification date(s) cpt/hcpc/service being disputed. Address, phone number and practice changes. Coordination of benefits (cob) employee assistance program (eap) medicaid disputes and appeals. Web find forms and applications for health care professionals and patients, all in one place. You may mail your request to:
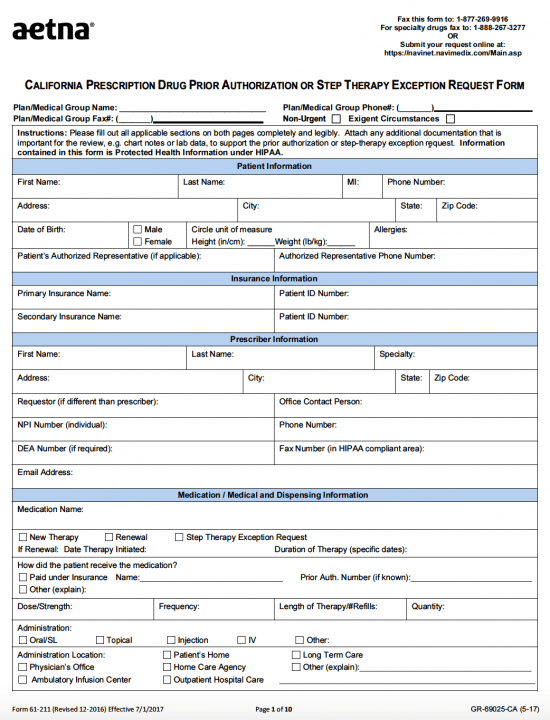
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls
Who may make a request: Or use our national fax number: Because aetna medicare (or one of our delegates) denied your request for coverage of a medical item or service or a medicare part b prescription drug, you have the right to ask us for an appeal of our decision. Web lexington, ky 40512 payment appeals for contracted provider requests.
Fillable Online aetna appeal form Fax Email Print pdfFiller
See how to get started 1 if you don't have creditable coverage for 63 days or more, you may have to pay a late enrollment penalty. Who may make a request: Providers in the aetna network have the right to appeal denied medical item or service authorizations or medicare part b prescription drug for members. Practitioner and provider compliant and.
You Must Submit Appeals Within 60 Days Of The Date Of Denial Notice.
Coordination of benefits (cob) employee assistance program (eap) medicaid disputes and appeals. You have 60 calendar days from the date of. Web lexington, ky 40512 payment appeals for contracted provider requests if you have a dispute around the rate used for payment you have received, please visit health care professional dispute and appeal process. If your complaint involves a broker or agent, be sure to include the name of the person when filing your grievance.
Web Complaints And Coverage Requests Please Come To Us If You Have A Concern About Your Coverage Or Care.
Web find forms and applications for health care professionals and patients, all in one place. Call us at the number on your member id card, or learn more first. Web helping patients to appeal denials on medicare authorization or precertification requests. See how to get started 1 if you don't have creditable coverage for 63 days or more, you may have to pay a late enrollment penalty.
Or Use Our National Fax Number:
Because aetna medicare (or one of our delegates) denied your request for coverage of a medical item or service or a medicare part b prescription drug, you have the right to ask us for an appeal of our decision. Practitioner and provider compliant and appeal request Providers in the aetna network have the right to appeal denied medical item or service authorizations or medicare part b prescription drug for members. You may mail your request to:
Make Sure To Include Any Information That Will Support Your Appeal.
This may be medical records, office notes, discharge. Who may make a request: Address, phone number and practice changes. Your doctor may ask us for an appeal on your behalf.