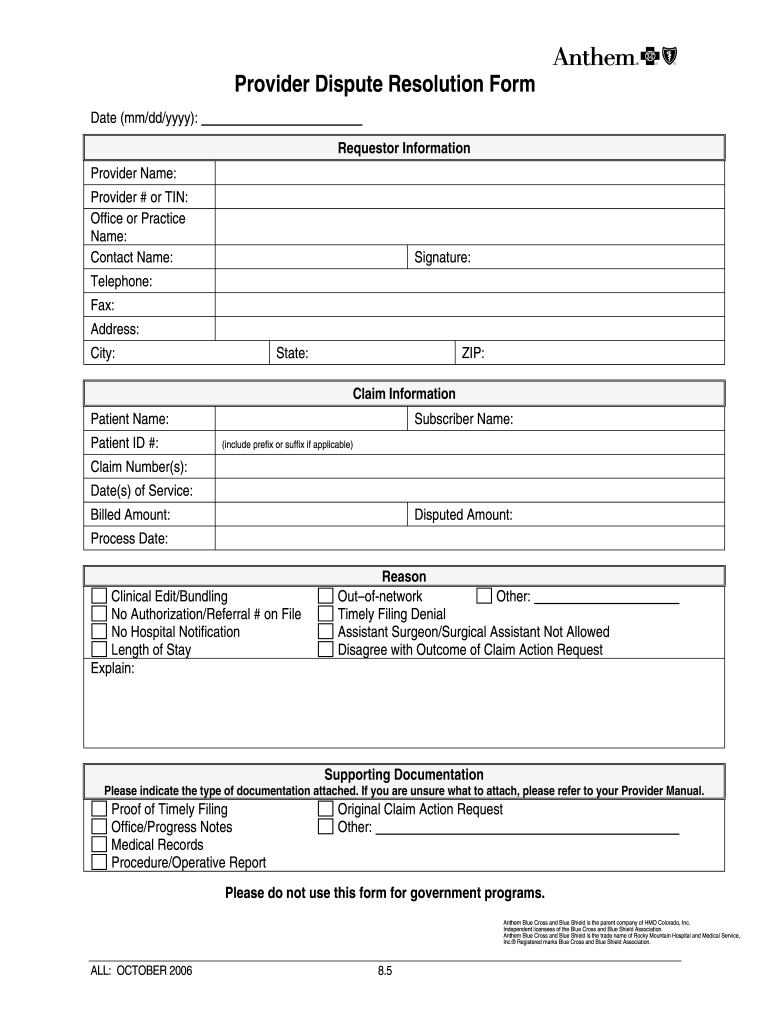
Anthem Provider Dispute Form
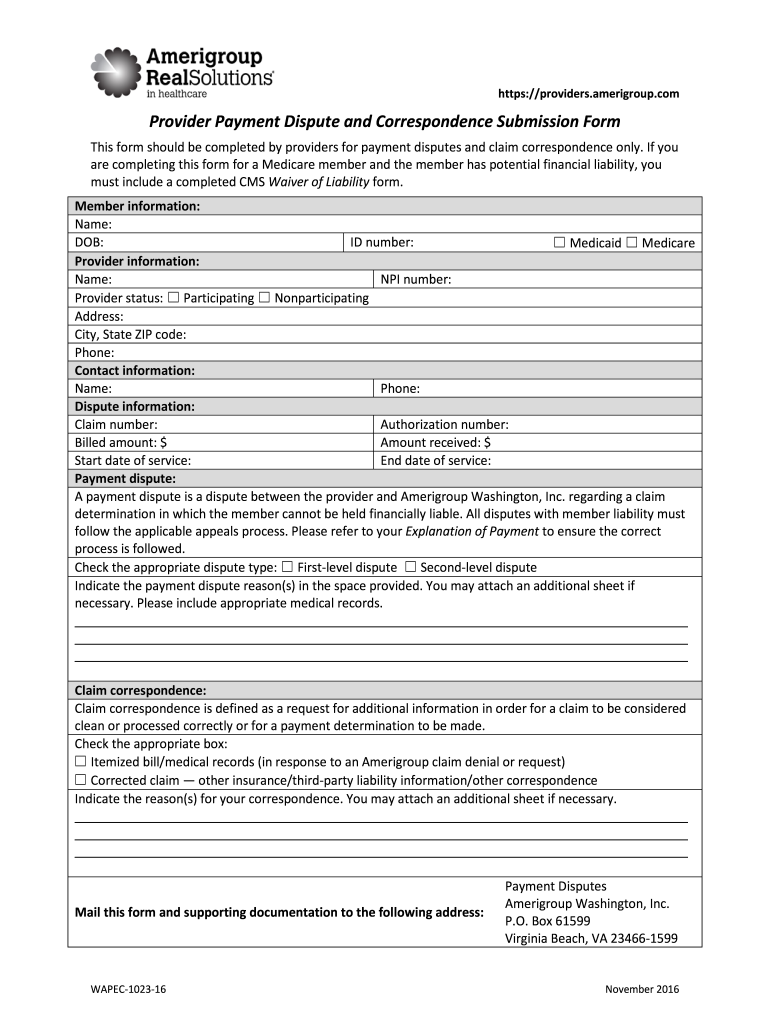
Anthem Provider Dispute Form - Clear claims connection to use clear. Web when submitting a claim payment dispute in writing, providers must include the claim information/ adjustment request 151 form and submit to: For more information on the claim dispute process,. Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient during the dispute process. Web this is the second step in the anthem healthkeepers plus provider payment dispute process. Select dispute the claim to begin the. Claims escalation, disputes, and appeals process. Contracted providers have 180 calendar days from the remit date; Please complete the form below. If you disagree with the outcome of the reconsideration, you may request an.
Web provider claim dispute process. Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider. Easily fill out pdf blank, edit, and sign them. Save or instantly send your ready documents. Select dispute the claim to begin the. A library of the forms most frequently used by health care professionals. Web your provider, or any other person you choose, may appeal for you. Easily fill out pdf blank, edit, and sign them. For more information on the claim dispute process,. Web to ensure timely and accurate processing of your request, please complete the payment dispute section below by checking the applicable determination provided on the anthem.
If you disagree with the outcome of the reconsideration, you may request an. Contracted providers have 180 calendar days from the remit date; National provider identifier (npi) number:. Looking for a form but don’t see it on this page? Web complete anthem provider dispute resolution request online with us legal forms. For more information on the claim dispute process,. Web provider forms & guides. Web when submitting a claim payment dispute in writing, providers must include the claim information/ adjustment request 151 form and submit to: Please complete the form below. Web what is the timeframe providers have to submit an appeal?
Anthem Blue Cross California Grievance Form Blue Cross Blue Shield
Web complete anthem provider dispute resolution request online with us legal forms. Easily fill out pdf blank, edit, and sign them. Web when submitting a claim payment dispute in writing, providers must include the claiminformation/ adjustment request form and submit to: Web to escalate, dispute, or appeal a claim, follow the steps in this document: If you disagree with the.
CA Anthem WPAPP004M 20132021 Fill and Sign Printable Template Online
Easily fill out pdf blank, edit, and sign them. Clear claims connection to use clear. National provider identifier (npi) number:. Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient during the dispute process. Web when submitting a claim payment dispute in writing, providers must include the claiminformation/ adjustment request form and submit.
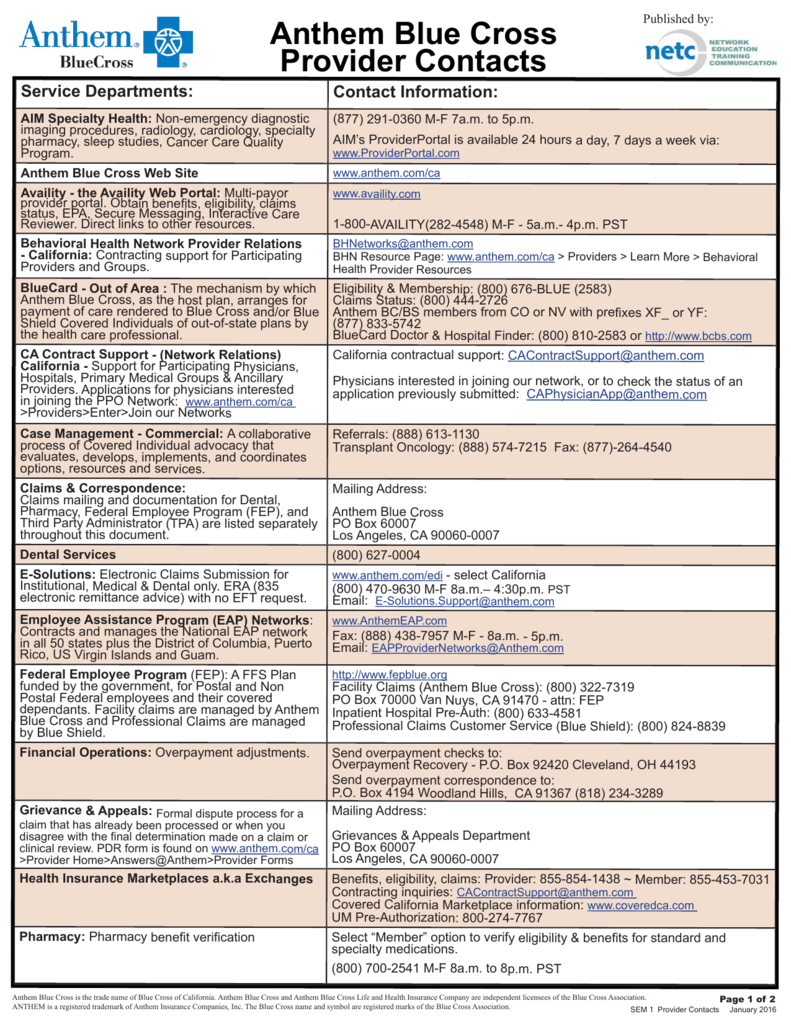
Anthem Blue Cross Provider Contacts
Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! Web complete anthem provider dispute resolution request online with us legal forms. Save or instantly send your ready documents. Web to escalate, dispute, or appeal a claim, follow the steps in this document: Web provider dispute resolution.
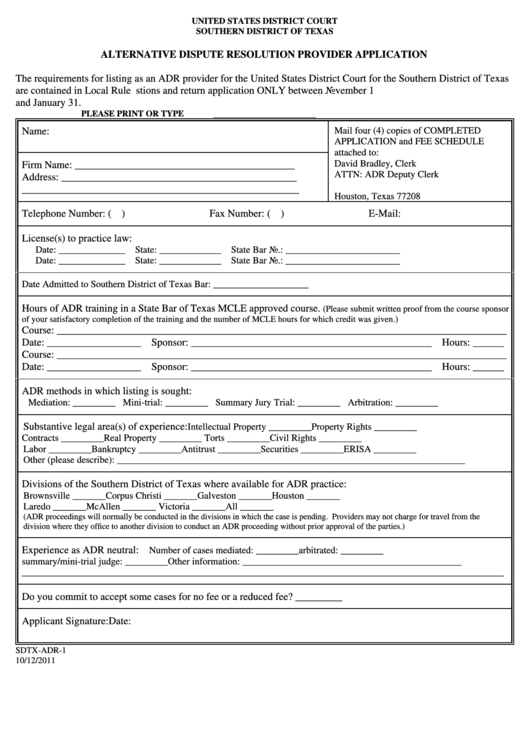
Alternative Dispute Resolution Provider Application Form 2011
Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient during the dispute process. Easily fill out pdf blank, edit, and sign them. Web provider forms & guides. Easily fill out pdf blank, edit, and sign them. Easily find and download forms, guides, and other related documentation that you need to do business.
Blank provider dispute form Fill out & sign online DocHub
Web to escalate, dispute, or appeal a claim, follow the steps in this document: Providers who disagree with the outcome of a claim can dispute that outcome when the claim is finalized. Web submit an inquiry and review the claims status detail page. Save or instantly send your ready documents. Web to ensure timely and accurate processing of your request,.
Anthem provider dispute form Fill out & sign online DocHub
Web what is the timeframe providers have to submit an appeal? If you ask someone to represent you, please give them a signed letter of consent to include with the appeal. Claims escalation, disputes, and appeals process. Web this is the second step in the anthem healthkeepers plus provider payment dispute process. Web use the provider dispute resolution request (pdr).
Indiana Medicaid Sterilization Consent Form Instructions 2022
Claims escalation, disputes, and appeals process. Contracted providers have 180 calendar days from the remit date; Web to ensure timely and accurate processing of your request, please complete the payment dispute section below by checking the applicable determination provided on the anthem. Save or instantly send your ready documents. If the claim is denied or final, there will be an.
Dispute Form Medicare Fill Online, Printable, Fillable, Blank pdfFiller
Clear claims connection to use clear. Anthem dispute resolution form & more fillable forms, register and subscribe now Get started on any device with our easy to use platform. Edit, sign and save anthem dispute resolution form. If you disagree with the outcome of the reconsideration, you may request an.
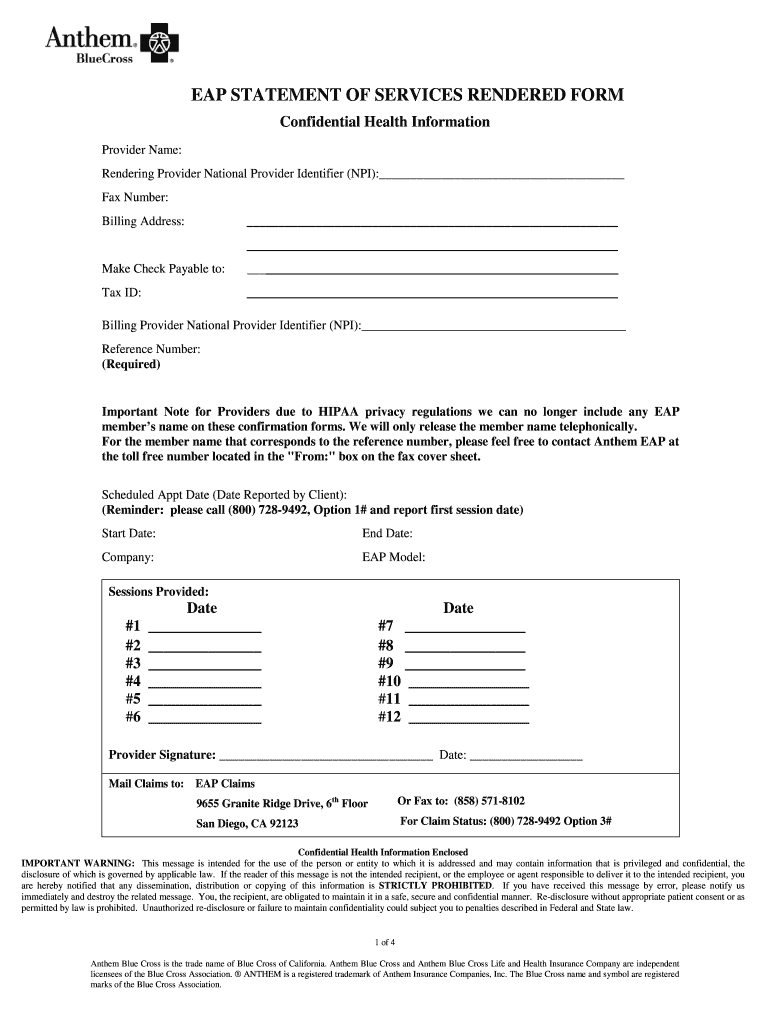
Eap Services Rendered Form Fill Out and Sign Printable PDF Template
If you disagree with the outcome of the reconsideration, you may request an. Web when submitting a claim payment dispute in writing, providers must include the claiminformation/ adjustment request form and submit to: Easily fill out pdf blank, edit, and sign them. Web provider forms & guides. Save or instantly send your ready documents.
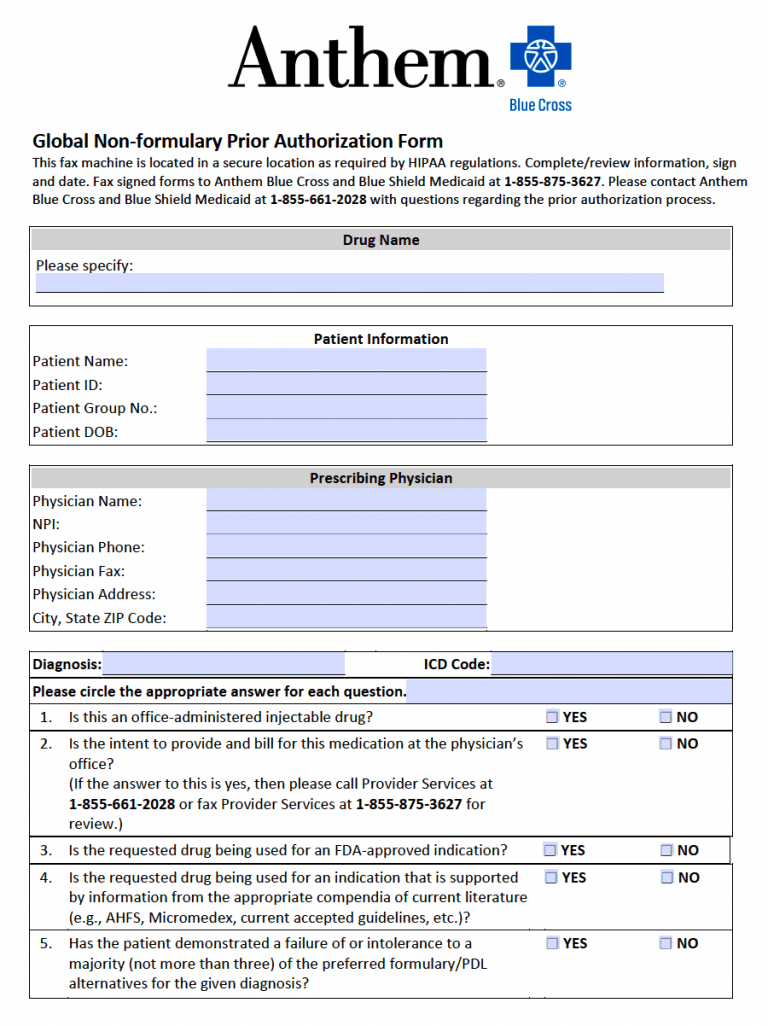
Free Anthem Blue Cross / Blue Shield Prior Prescription (Rx
Anthem dispute resolution form & more fillable forms, register and subscribe now Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient during the dispute process. Web this is the second step in the anthem healthkeepers plus provider payment dispute process. Web when submitting a claim payment dispute in writing, providers must include.
Easily Fill Out Pdf Blank, Edit, And Sign Them.
If you disagree with the outcome of the reconsideration, you may request an. Select dispute the claim to begin the. Web to escalate, dispute, or appeal a claim, follow the steps in this document: Web your provider, or any other person you choose, may appeal for you.
Save Or Instantly Send Your Ready Documents.
Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! Anthem dispute resolution form & more fillable forms, register and subscribe now Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider. Web provider claim dispute process.
National Provider Identifier (Npi) Number:.
Please complete the form below. Web when submitting a claim payment dispute in writing, providers must include the claim information/ adjustment request 151 form and submit to: Easily fill out pdf blank, edit, and sign them. Providers who disagree with the outcome of a claim can dispute that outcome when the claim is finalized.
Contracted Providers Have 180 Calendar Days From The Remit Date;
Claims escalation, disputes, and appeals process. Web when submitting a claim payment dispute in writing, providers must include the claiminformation/ adjustment request form and submit to: Clear claims connection to use clear. Looking for a form but don’t see it on this page?