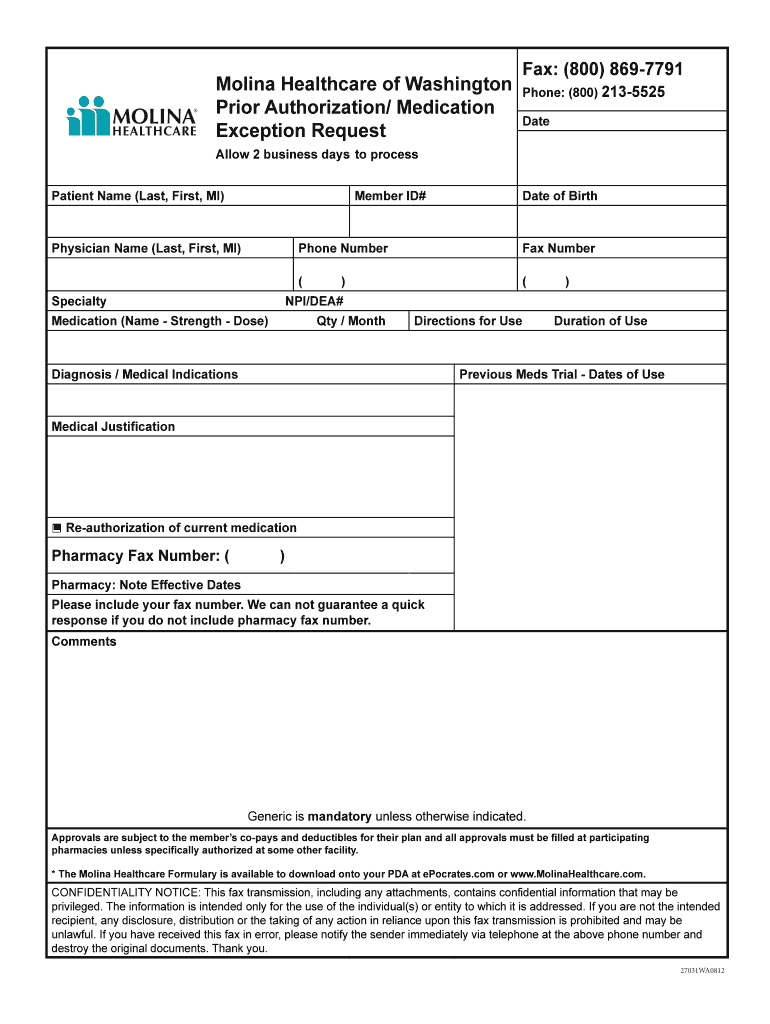
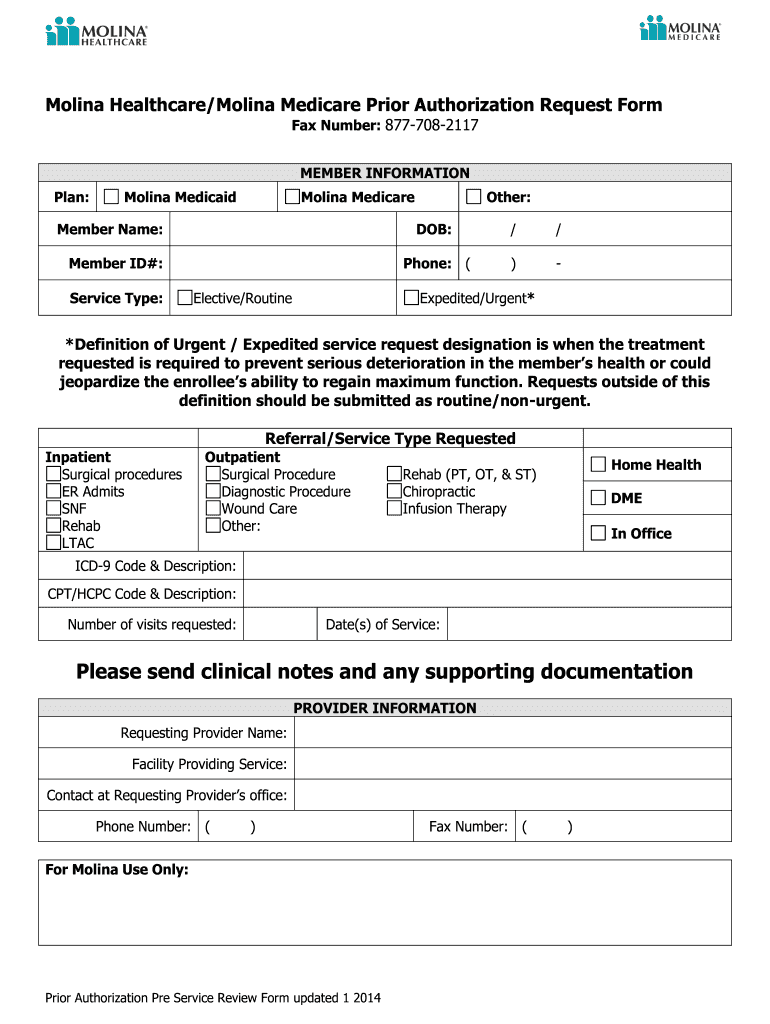
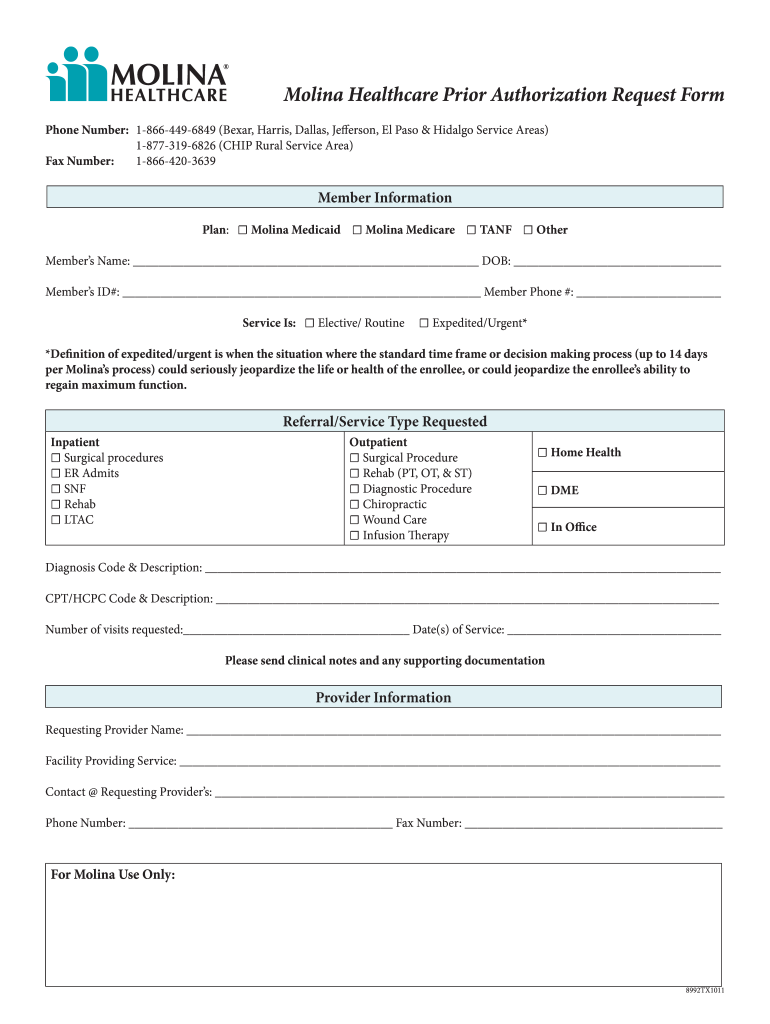
Molina Medicaid Prior Auth Form
Molina Medicaid Prior Auth Form - Q1 2022 medicaid pa guide/request form effective 01.01.2022 molina® healthcare, inc. Web on the universal prior authorization form and include a copy of the individual family service plan. Web molina healthcare medicaid prior authorization request. Molina healthcare prior authorization request form and instructions. • cosmetic, plastic and reconstructive procedures {in any setting): Mississippican prior authorization request form effective 10.01.18 53593ms190903. Web prior authorization lookup tool. Prior authorization request contact information. Refer to number(s) above fax number: A molina healthcare prior authorization form is submitted by a physician to request.
Applied behavior analysis (aba) therapy prior. Web pharmacy point of sale claims must be submitted to cvs prior authorization is required as noted on the pdl or for fda approved drugs not found on the pdl (excluding non. Q1 2022 medicaid pa guide/request form effective 01.01.2022 molina® healthcare, inc. Web prior authorization lookup tool. Web molina healthcare medicaid prior authorization request. Refer to number(s) above fax number: Web molina healthcare prior (rx) authorization form. Mississippican prior authorization request form effective 10.01.18 53593ms190903. Molina healthcare contact information prior authorizations: Web on the universal prior authorization form and include a copy of the individual family service plan.
Molina healthcare prior authorization request form and instructions. For pharmacy prior authorization forms, please visit the washington drug formulary page. Web on the universal prior authorization form and include a copy of the individual family service plan. Learn more about the appeal process. Molina healthcare prior authorization request form and instructions. Web molina healthcare medicaid prior authorization request. Refer to number(s) above fax number: The quickest option for checking the status of a request is through our telephonic self. Web appeal if a prior authorization request is denied and the reconsideration is denied, your provider can submit an appeal. Web prior authorization lookup tool.
Molina Authorization Form Fill Online, Printable, Fillable, Blank
Web appeal if a prior authorization request is denied and the reconsideration is denied, your provider can submit an appeal. Molina healthcare prior authorization request form and instructions. Web molina healthcare medicaid prior authorization request. Applied behavior analysis (aba) therapy prior. Web pharmacy point of sale claims must be submitted to cvs prior authorization is required as noted on the.
Molina Prior Authorization Form Fill Out and Sign Printable PDF
Molina healthcare prior authorization request form and instructions. Web prior authorization lookup tool. Web authorizationsubmissionandstatus • claimssubmissionandstatus member eligibility • downloadfrequentlyusedforms provider directory • nurse advice line report molina. Web molina healthcare prior (rx) authorization form. The quickest option for checking the status of a request is through our telephonic.
Molina Prior Authorization Form 2021 Fill Online, Printable, Fillable
The fastest route for prior authorization is submission via fax. Applied behavior analysis (aba) therapy prior. 01/01/2022 refer to molina’s provider website or. Mississippican prior authorization request form effective 10.01.18 53593ms190903. Web authorizationsubmissionandstatus • claimssubmissionandstatus member eligibility • downloadfrequentlyusedforms provider directory • nurse advice line report molina.
Prior Authorization YouTube
Molina healthcare prior authorization request form and instructions. Prior authorization request contact information. The fastest route for prior authorization is submission via fax. Web molina healthcare prior (rx) authorization form. Web prior authorization lookup tool.
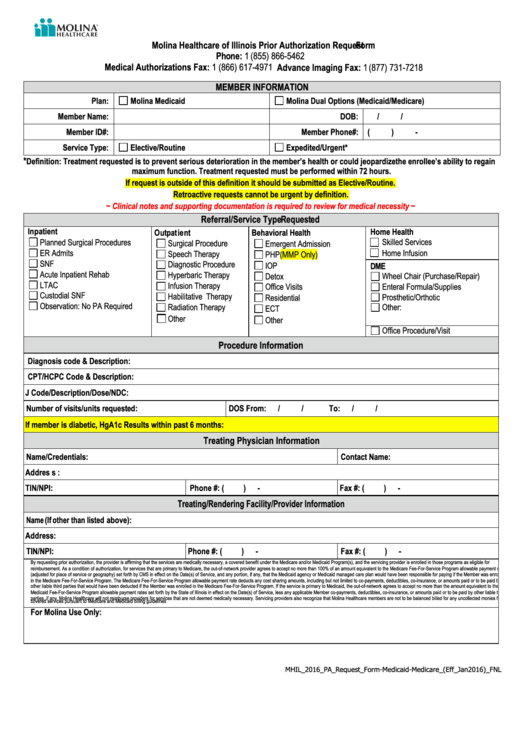
Molina Healthcare Of Illinois Prior Authorization Request printable pdf
For pharmacy prior authorization forms, please visit the washington drug formulary page. The fastest route for prior authorization is submission via fax. Web molina complete care prior authorization request form member information line of business: The quickest option for checking the status of a request is through our telephonic. Molina healthcare contact information prior authorizations:
Anthem Medicare Advantage Disenrollment Form Form Resume Examples
For pharmacy prior authorization forms, please visit the washington drug formulary page. ☐ medicaid ☐ marketplace ☐ medicare. Molina healthcare prior authorization request form and instructions. The quickest option for checking the status of a request is through our telephonic. Molina healthcare prior authorization request form and instructions.
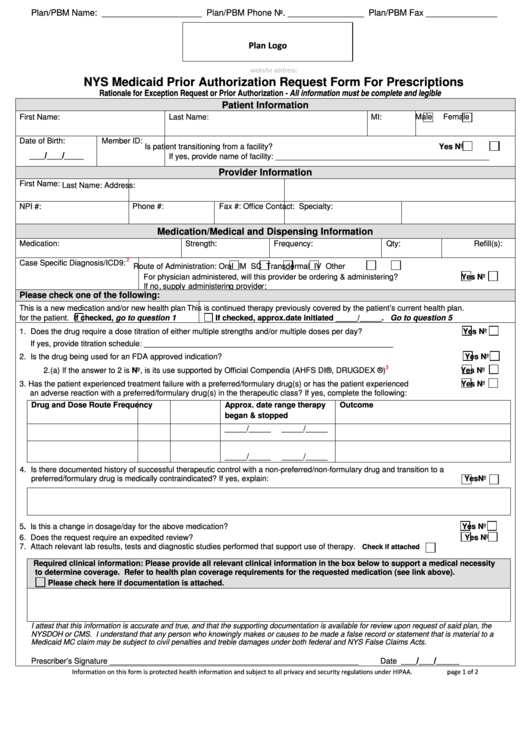
Fillable Nys Medicaid Prior Authorization Request Form For
• cosmetic, plastic and reconstructive procedures {in any setting): ☐ medicaid ☐ marketplace ☐ medicare. The quickest option for checking the status of a request is through our telephonic. Prior authorization request contact information. Molina healthcare contact information prior authorizations:
WA Molina Healthcare Behavioral Health Authorization/Notification Form
Refer to number(s) above fax number: Mississippican prior authorization request form effective 10.01.18 53593ms190903. The quickest option for checking the status of a request is through our telephonic self. Web molina healthcare prior (rx) authorization form. The fastest route for prior authorization is submission via fax.
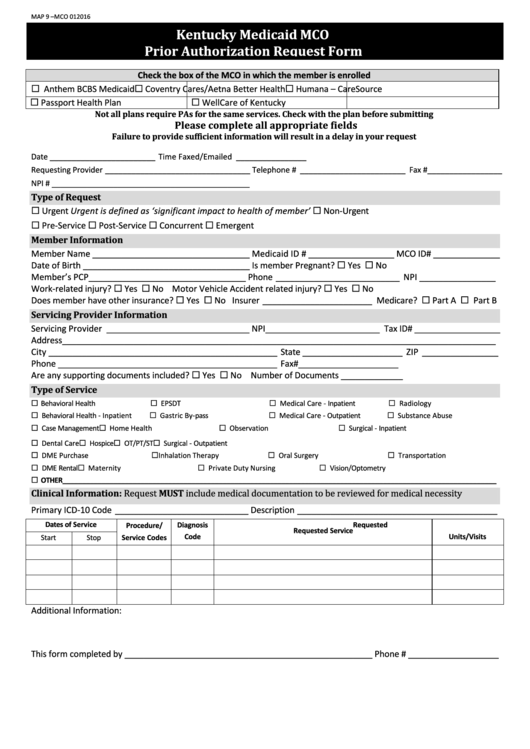
Fillable Kentucky Medicaid Mco Prior Authorization Request Form
01/01/2022 refer to molina’s provider website or. Refer to number(s) above fax number: Molina healthcare prior authorization request form and instructions. Web on the universal prior authorization form and include a copy of the individual family service plan. Molina healthcare contact information prior authorizations:
Molina Drug Prior Authorization Fill Online, Printable, Fillable
• cosmetic, plastic and reconstructive procedures {in any setting): 01/01/2022 refer to molina’s provider website or. Web on the universal prior authorization form and include a copy of the individual family service plan. Web molina healthcare prior (rx) authorization form. Refer to number(s) above fax number:
The Quickest Option For Checking The Status Of A Request Is Through Our Telephonic Self.
☐ medicaid ☐ marketplace ☐ medicare. Web prior authorization lookup tool. Applied behavior analysis (aba) therapy prior. Q1 2022 medicaid pa guide/request form effective 01.01.2022 molina® healthcare, inc.
Web Molina Healthcare Medicaid Prior Authorization Request.
Molina healthcare prior authorization request form and instructions. The quickest option for checking the status of a request is through our telephonic. The fastest route for prior authorization is submission via fax. Learn more about the appeal process.
Web Appeal If A Prior Authorization Request Is Denied And The Reconsideration Is Denied, Your Provider Can Submit An Appeal.
Web prior authorization lookup tool. For pharmacy prior authorization forms, please visit the washington drug formulary page. Mississippican prior authorization request form effective 10.01.18 53593ms190903. Web molina complete care prior authorization request form member information line of business:
Web Molina Healthcare Prior (Rx) Authorization Form.
• cosmetic, plastic and reconstructive procedures {in any setting): Molina healthcare prior authorization request form and instructions. Web pharmacy point of sale claims must be submitted to cvs prior authorization is required as noted on the pdl or for fda approved drugs not found on the pdl (excluding non. Web authorizationsubmissionandstatus • claimssubmissionandstatus member eligibility • downloadfrequentlyusedforms provider directory • nurse advice line report molina.