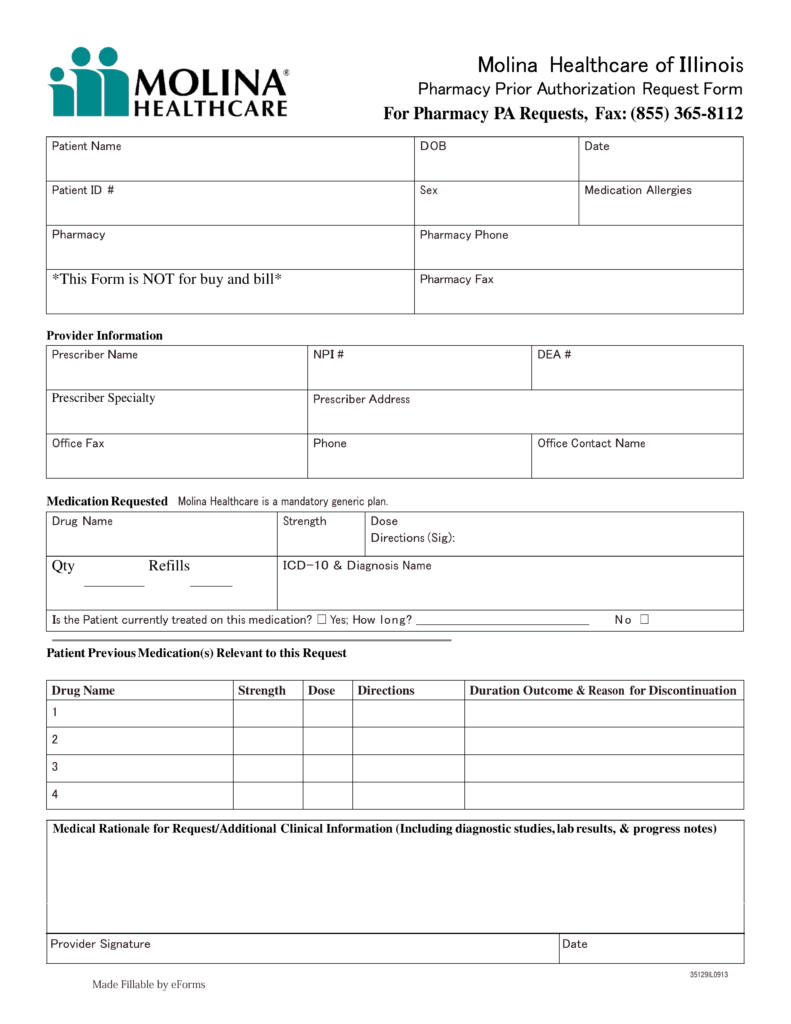
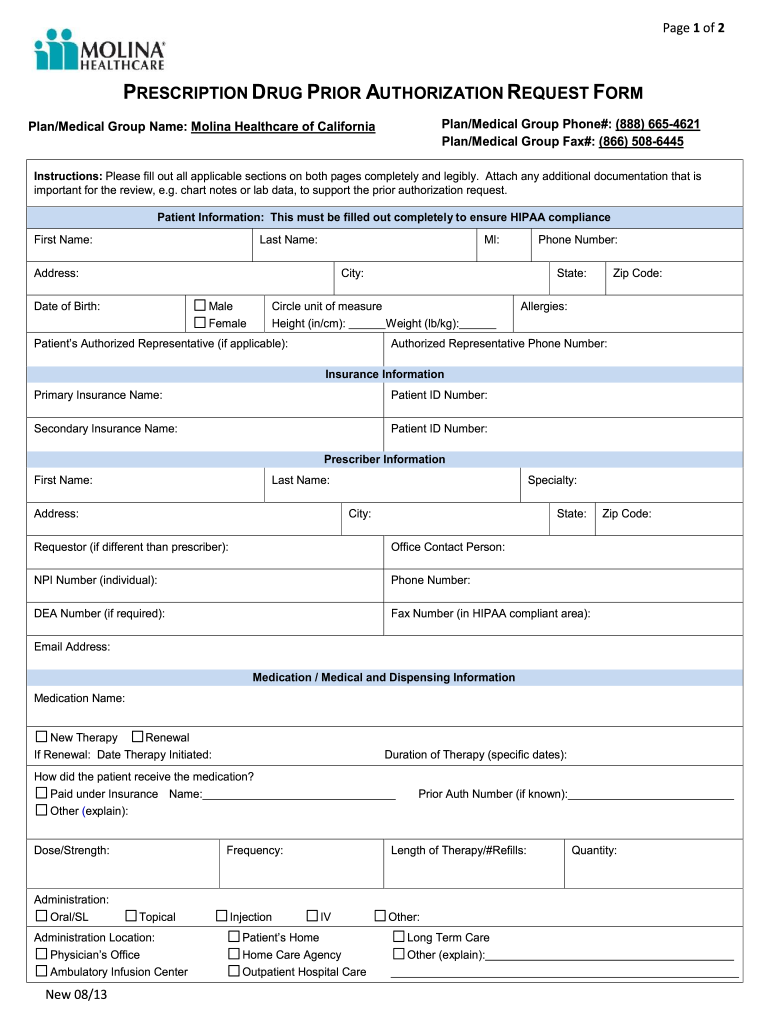
Molina Pharmacy Prior Auth Form
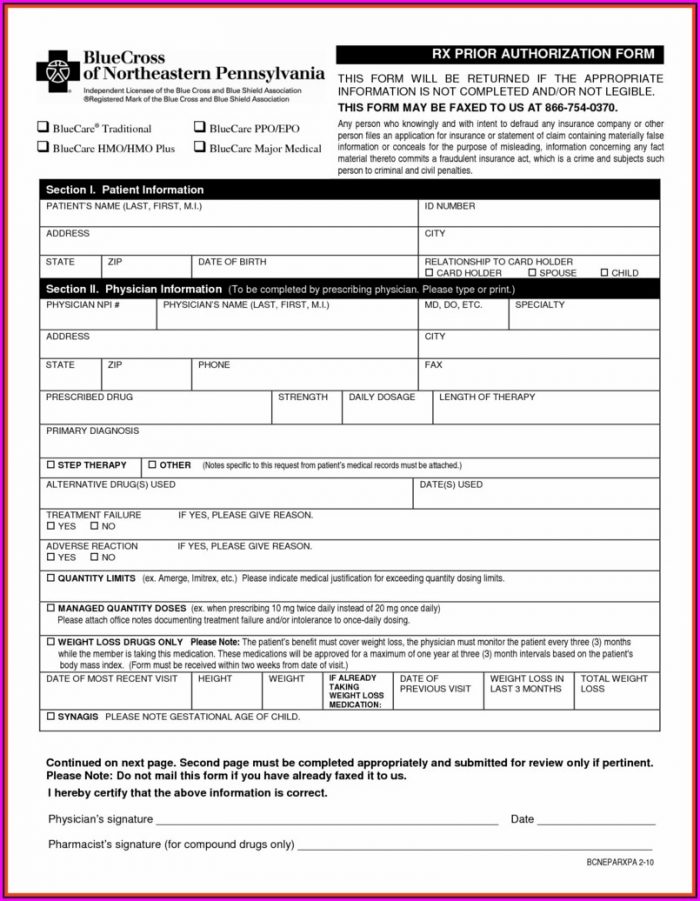
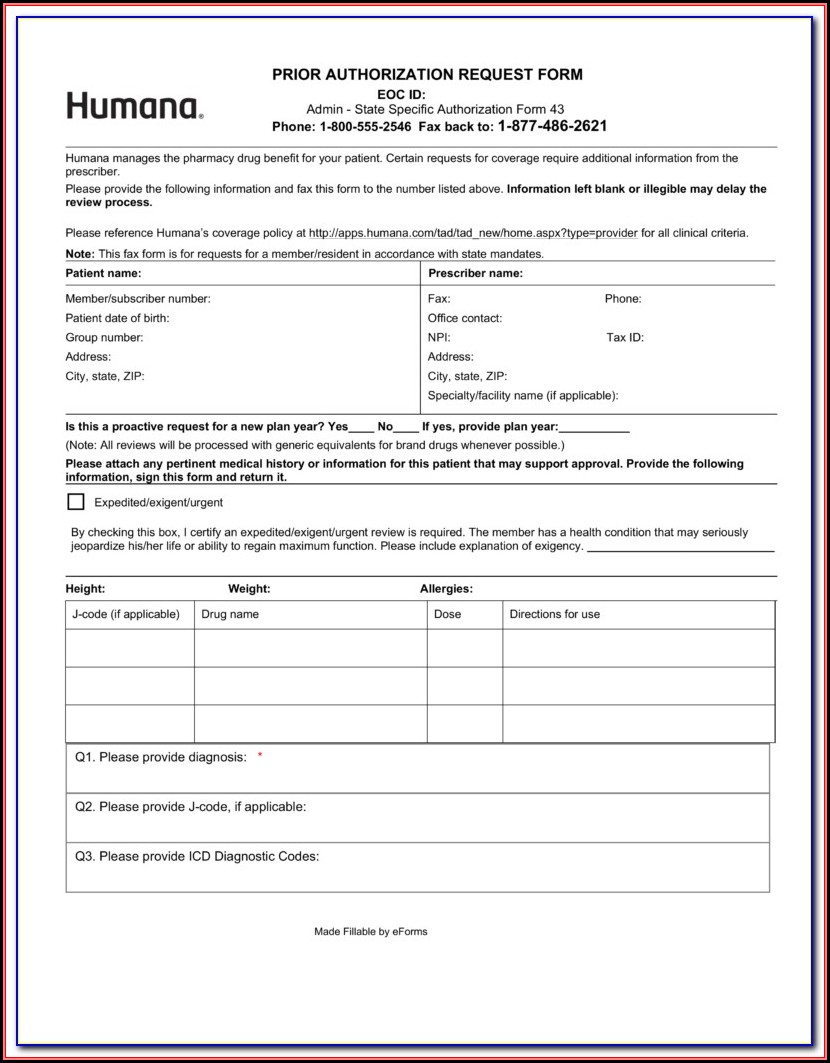
Molina Pharmacy Prior Auth Form - Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Prior authorization form and formulary booklet may be found at. Web manage your rx and get help when you need it. The quickest option for checking the status of a request is through our telephonic. Web follow these steps for efficient processing of your pharmacy prior authorization requests: Previous medications tried and dates of use: 2023 medicaid pa guide/request form (vendors). Molina healthcare prior authorization request form and instructions. Web molina healthcare of washington prior authorization/ medication exception request allow 2 business days to process fax: Universal synagis prior authorization form.
2023 medicaid pa guide/request form (vendors). The quickest option for checking the status of a request is through our telephonic. Web follow these steps for efficient processing of your pharmacy prior authorization requests: Web the authorization process, please include the following information when requesting these types. Molina healthcare prior authorization request form and instructions. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions,. Prior authorization request contact information. The fastest route for prior authorization is submission via fax. ☐ medicaid ☐ marketplace ☐ medicare. ☐ pharmacy pharmacy (1022) please add codes being requested.
2023 medicaid pa guide/request form (vendors). Web prior authorization is not a guarantee of payment for services. Complete the cvs caremark form: You may also fax in. The fastest route for prior authorization is submission via fax. ☐ pharmacy pharmacy (1022) please add codes being requested. Web providers are able to complete prior authorizations online via the following link: Previous medications tried and dates of use: Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Universal synagis prior authorization form.
Prior Authorization Form For Molina Medicare Universal Network
Electronic prior authorization information texas standardized prior. You may also fax in. Web manage your rx and get help when you need it. Molina healthcare prior authorization request form and instructions. Web providers are able to complete prior authorizations online via the following link:
Molina Healthcare Medication Prior Authorization/Exceptions Request
Web follow these steps for efficient processing of your pharmacy prior authorization requests: Web prior authorization is not a guarantee of payment for services. Complete the cvs caremark form: Web molina complete care prior authorization request form member information line of business: Web molina healthcare of washington prior authorization/ medication exception request allow 2 business days to process fax:
FL Molina Healthcare Medication Prior Authorization/Exceptions Request
Universal synagis prior authorization form. Web for medicare part b drug provider administered drug therapies, please direct prior authorization requests to novologixvia the molina provider portal. You may also fax in. ☐ medicaid ☐ marketplace ☐ medicare. Web pharmacy prior authorization forms.
Molina Medicare Medication Prior Authorization Form Form Resume
The quickest option for checking the status of a request is through our telephonic. Web prior authorization is not a guarantee of payment for services. Web providers are able to complete prior authorizations online via the following link: The fastest route for prior authorization is submission via fax. ☐ pharmacy pharmacy (1022) please add codes being requested.
Molina Medicare Medication Prior Authorization Form Form Resume
Prior authorization request contact information. Web molina complete care prior authorization request form member information line of business: Web molina healthcare of washington prior authorization/ medication exception request allow 2 business days to process fax: Web prior authorization lookup tool. You may also fax in.
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
Web follow these steps for efficient processing of your pharmacy prior authorization requests: Universal synagis prior authorization form. Web prior authorization lookup tool. Web manage your rx and get help when you need it. Previous medications tried and dates of use:
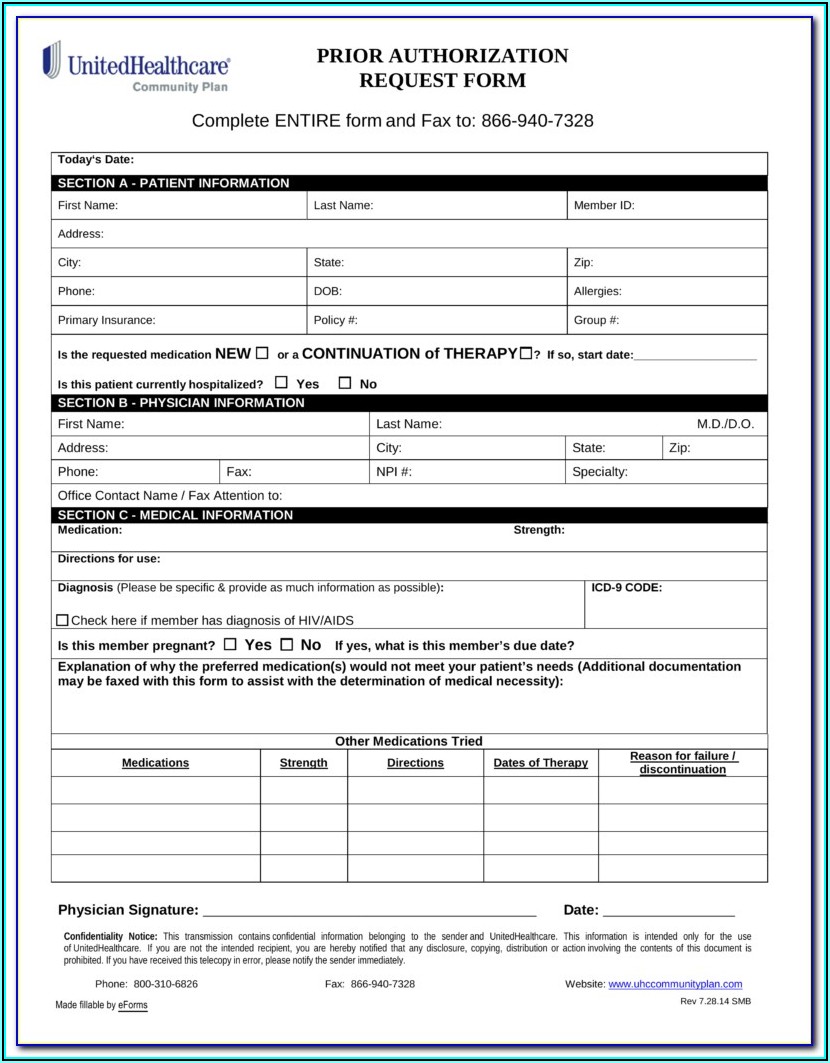
Drug Authorization Form Fill Out and Sign Printable PDF Template
Complete the cvs caremark form: Web manage your rx and get help when you need it. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions,. Molina healthcare prior authorization request form and instructions. Universal synagis prior authorization form.
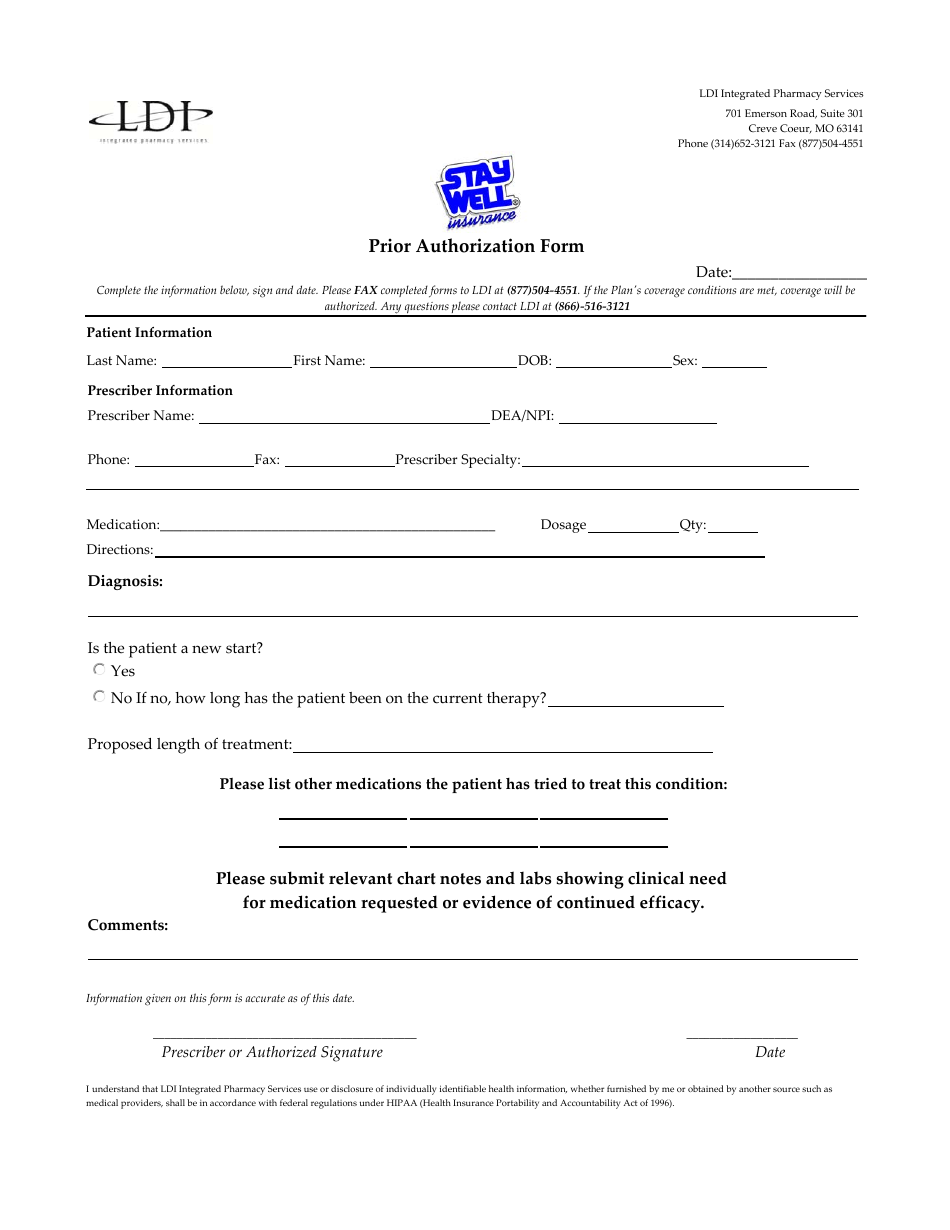
Missouri Prior Authorization Form Ldi Integrated Pharmacy Services
Universal synagis prior authorization form. Web manage your rx and get help when you need it. Web for medicare part b drug provider administered drug therapies, please direct prior authorization requests to novologixvia the molina provider portal. Web molina complete care prior authorization request form member information line of business: Molina healthcare prior authorization request form and instructions.
WA Molina Healthcare Behavioral Health Authorization/Notification Form
Web for medicare part b drug provider administered drug therapies, please direct prior authorization requests to novologixvia the molina provider portal. Complete the cvs caremark form: The fastest route for prior authorization is submission via fax. Previous medications tried and dates of use: Prior authorization request contact information.
Molina Medicare Medication Prior Authorization Form Form Resume
Web follow these steps for efficient processing of your pharmacy prior authorization requests: 2023 medicaid pa guide/request form (vendors). Web manage your rx and get help when you need it. Complete the cvs caremark form: Previous medications tried and dates of use:
Web Pharmacy Prior Authorization Forms.
You may also fax in. Web for medicare part b drug provider administered drug therapies, please direct prior authorization requests to novologixvia the molina provider portal. The quickest option for checking the status of a request is through our telephonic. ☐ medicaid ☐ marketplace ☐ medicare.
Previous Medications Tried And Dates Of Use:
Web prior authorization lookup tool. Web follow these steps for efficient processing of your pharmacy prior authorization requests: Web molina healthcare of washington prior authorization/ medication exception request allow 2 business days to process fax: Molina healthcare prior authorization request form and instructions.
The Fastest Route For Prior Authorization Is Submission Via Fax.
Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Prior authorization form and formulary booklet may be found at. Web manage your rx and get help when you need it. ☐ pharmacy pharmacy (1022) please add codes being requested.
Payment Is Made In Accordance With A Determination Of The Member’s Eligibility, Benefit Limitation/Exclusions,.
Web prior authorization is not a guarantee of payment for services. Web the authorization process, please include the following information when requesting these types. Web molina complete care prior authorization request form member information line of business: Prior authorization request contact information.