Standard Prior Authorization Form
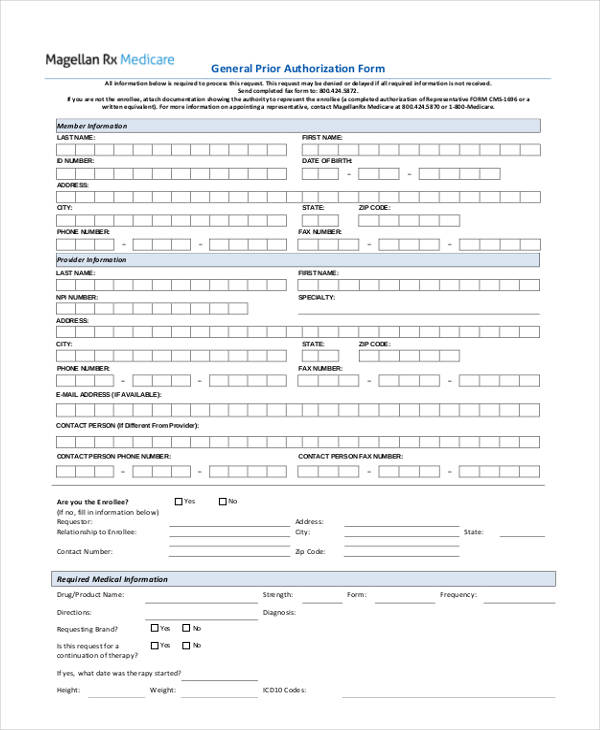
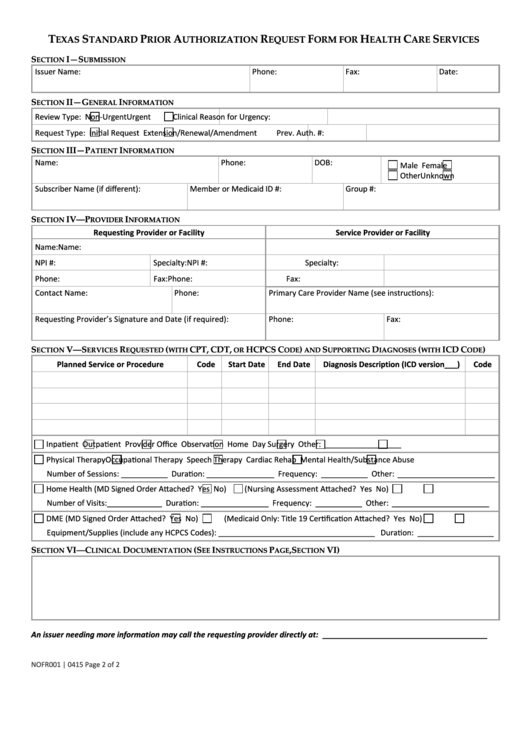
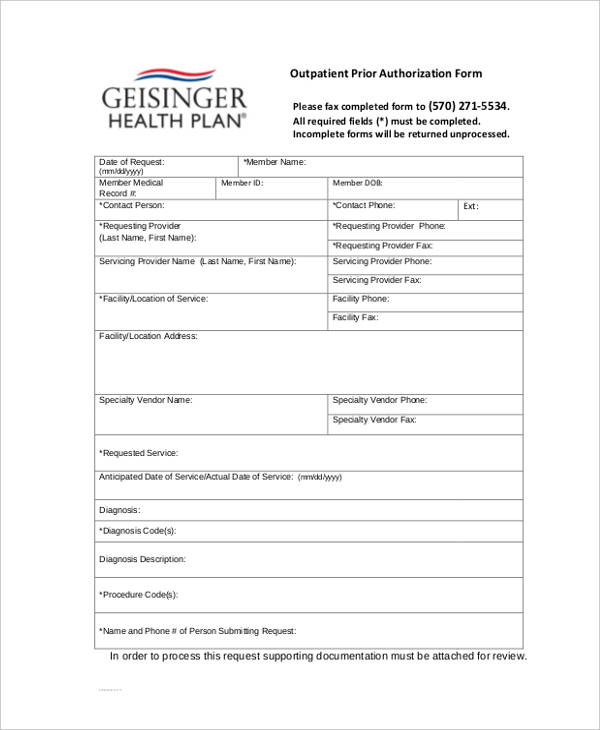
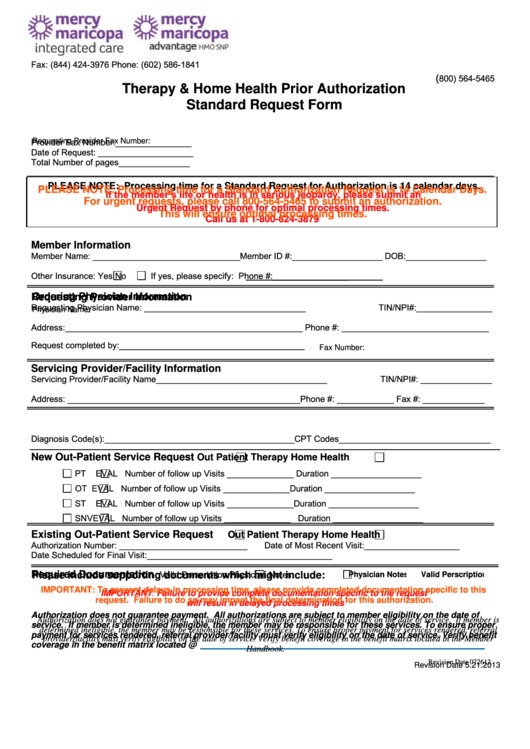
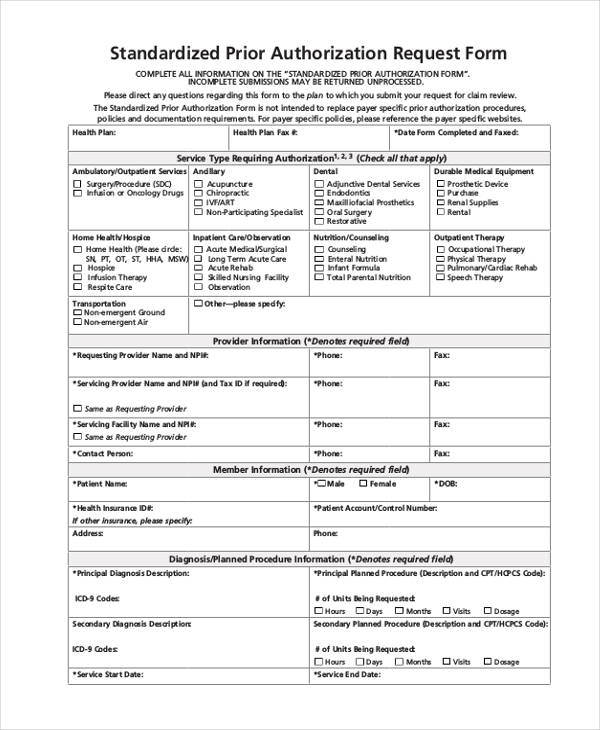
Standard Prior Authorization Form - ☐ initial request continuation/renewal request reason for request (check all that apply): Web electronically, through the issuer’s portal, to request prior authorization of a health care service. The prior authorization request form is for use with the following service types: The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. Web what is the purpose of the form? An attestation was added as a certification that any request submitted with the expedited timeframe meets the cms criteria. 4) request a guarantee of payment; It is intended to assist providers by streamlining the data submission process for selected services that. Web massachusetts standard form for medication prior authorization requests *some plans might not accept this form for medicare or medicaid requests. ☐ prior authorization, step therapy, formulary exception
The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. The new form is now available for download on the cca website. Web standardized prior authorization request form standardized prior authorization request form 3 this form does not replace payer specific prior authorization requirements. An attestation was added as a certification that any request submitted with the expedited timeframe meets the cms criteria. ☐ initial request continuation/renewal request reason for request (check all that apply): It is intended to assist providers by streamlining the data submission process for selected services that. Web cca has a new standardized prior authorization form to ensure that minimal processing information is captured. Web ohio department of medicaid | 50 west town street, suite 400, columbus, ohio 43215. Web what is the purpose of the form? Web massachusetts standard form for medication prior authorization requests *some plans might not accept this form for medicare or medicaid requests.
Do not use this form to: Web cca has a new standardized prior authorization form to ensure that minimal processing information is captured. ☐ initial request continuation/renewal request reason for request (check all that apply): ☐ prior authorization, step therapy, formulary exception It is intended to assist providers by streamlining the data submission process for selected services that. Web standardized prior authorization request form standardized prior authorization request form 3 this form does not replace payer specific prior authorization requirements. The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. This form is being used for: Web ohio department of medicaid | 50 west town street, suite 400, columbus, ohio 43215. 4) request a guarantee of payment;
FREE 13+ Prior Authorization Forms in PDF MS Word
Web massachusetts standard form for medication prior authorization requests *some plans might not accept this form for medicare or medicaid requests. ☐ prior authorization, step therapy, formulary exception The new form is now available for download on the cca website. This form is being used for: 4) request a guarantee of payment;
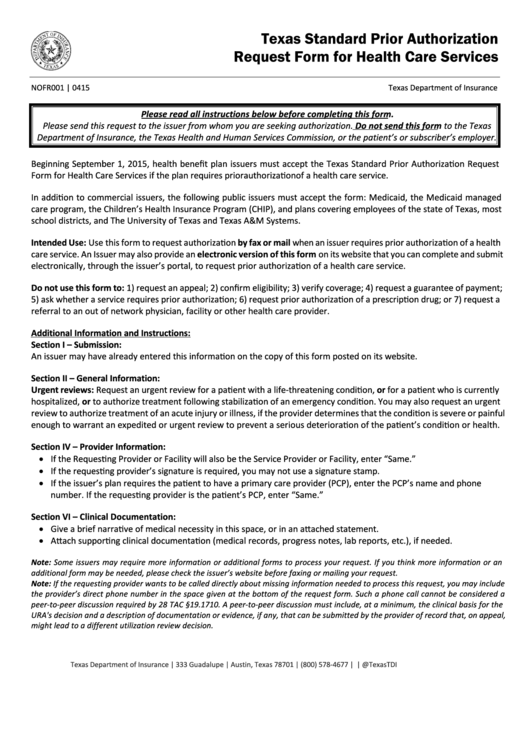
Fillable Texas Standard Prior Authorization Request Form For Health
Web standardized prior authorization request form standardized prior authorization request form 3 this form does not replace payer specific prior authorization requirements. Web electronically, through the issuer’s portal, to request prior authorization of a health care service. Web the standardized prior authorization form is intended to be used to submit prior authorization requests by fax. The prior authorization request form.
FREE 13+ Prior Authorization Forms in PDF MS Word
The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. Web massachusetts standard form for medication prior authorization requests *some plans might not accept this form for medicare or medicaid requests. An attestation was added as a certification that any request submitted with the expedited timeframe meets the cms criteria. Web electronically, through.
Fillable Therapy & Home Health Prior Authorization Standard Request
Requesting providers should attach all pertinent medical documentation to support the request and submit to cca for review. The new form is now available for download on the cca website. This form is being used for: Web cca has a new standardized prior authorization form to ensure that minimal processing information is captured. Web what is the purpose of the.
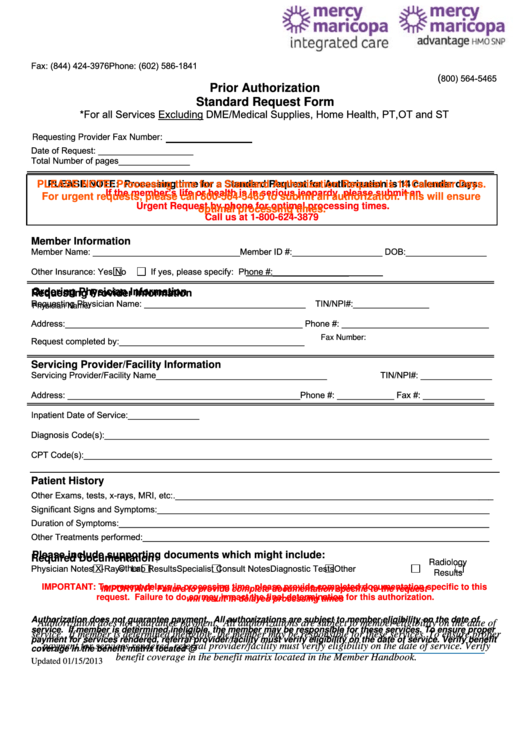
Fillable Prior Authorization Standard Request Form printable pdf download
4) request a guarantee of payment; An attestation was added as a certification that any request submitted with the expedited timeframe meets the cms criteria. Do not use this form to: Web cca has a new standardized prior authorization form to ensure that minimal processing information is captured. This form is being used for:
FREE 13+ Prior Authorization Forms in PDF MS Word
The prior authorization request form is for use with the following service types: Web electronically, through the issuer’s portal, to request prior authorization of a health care service. ☐ initial request continuation/renewal request reason for request (check all that apply): This form is being used for: Requesting providers should attach all pertinent medical documentation to support the request and submit.
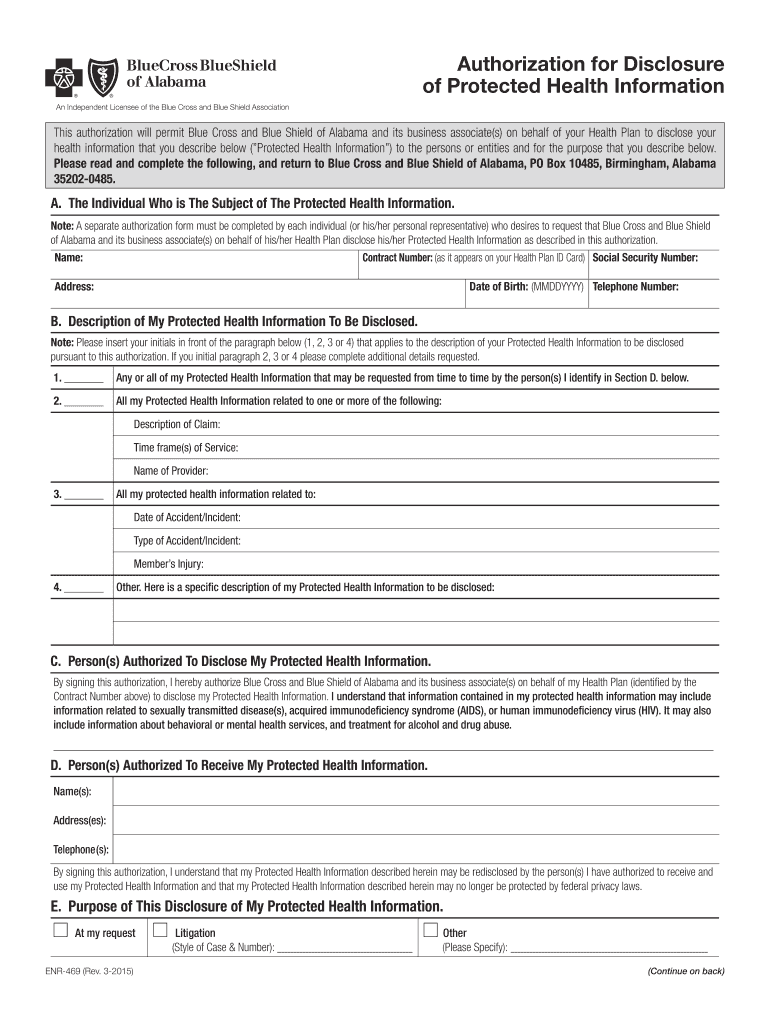
20152022 AL BCBS Form ENR469 Fill Online, Printable, Fillable, Blank
Do not use this form to: ☐ prior authorization, step therapy, formulary exception This form is being used for: Requesting providers should attach all pertinent medical documentation to support the request and submit to cca for review. Web cca has a new standardized prior authorization form to ensure that minimal processing information is captured.
Fillable Texas Standard Prior Authorization Request Form For Health
Requesting providers should attach all pertinent medical documentation to support the request and submit to cca for review. It is intended to assist providers by streamlining the data submission process for selected services that. 4) request a guarantee of payment; An attestation was added as a certification that any request submitted with the expedited timeframe meets the cms criteria. The.
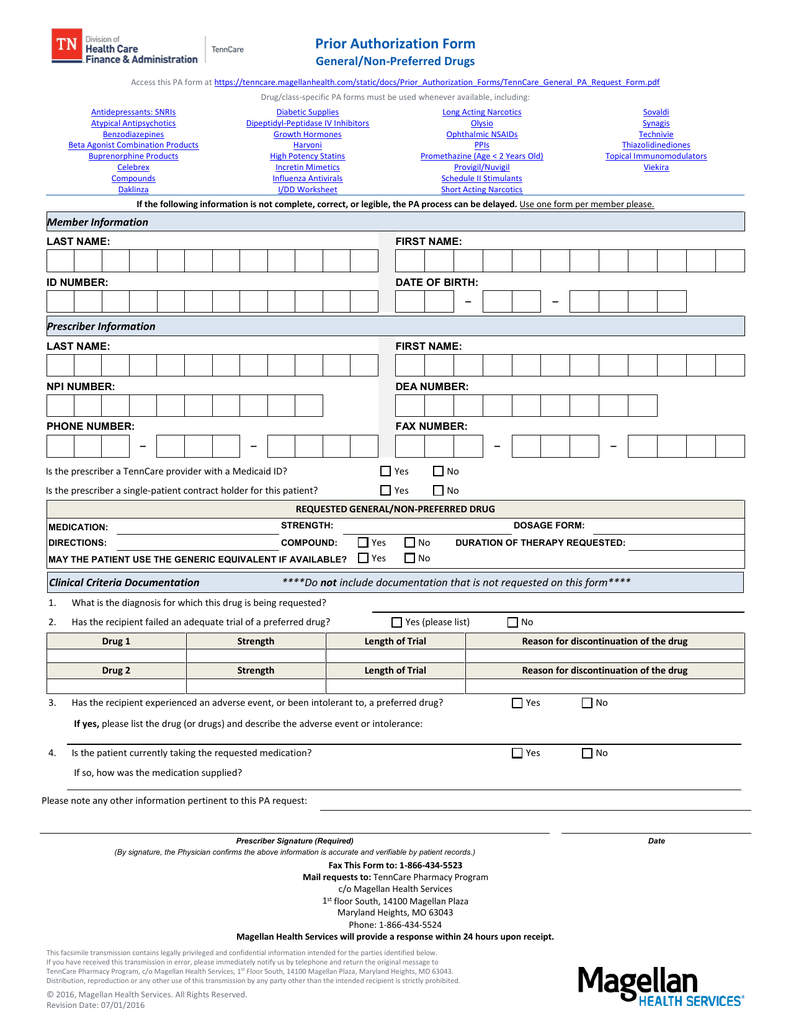
Prior Authorization Form
☐ prior authorization, step therapy, formulary exception Web ohio department of medicaid | 50 west town street, suite 400, columbus, ohio 43215. 4) request a guarantee of payment; The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. Requesting providers should attach all pertinent medical documentation to support the request and submit to.
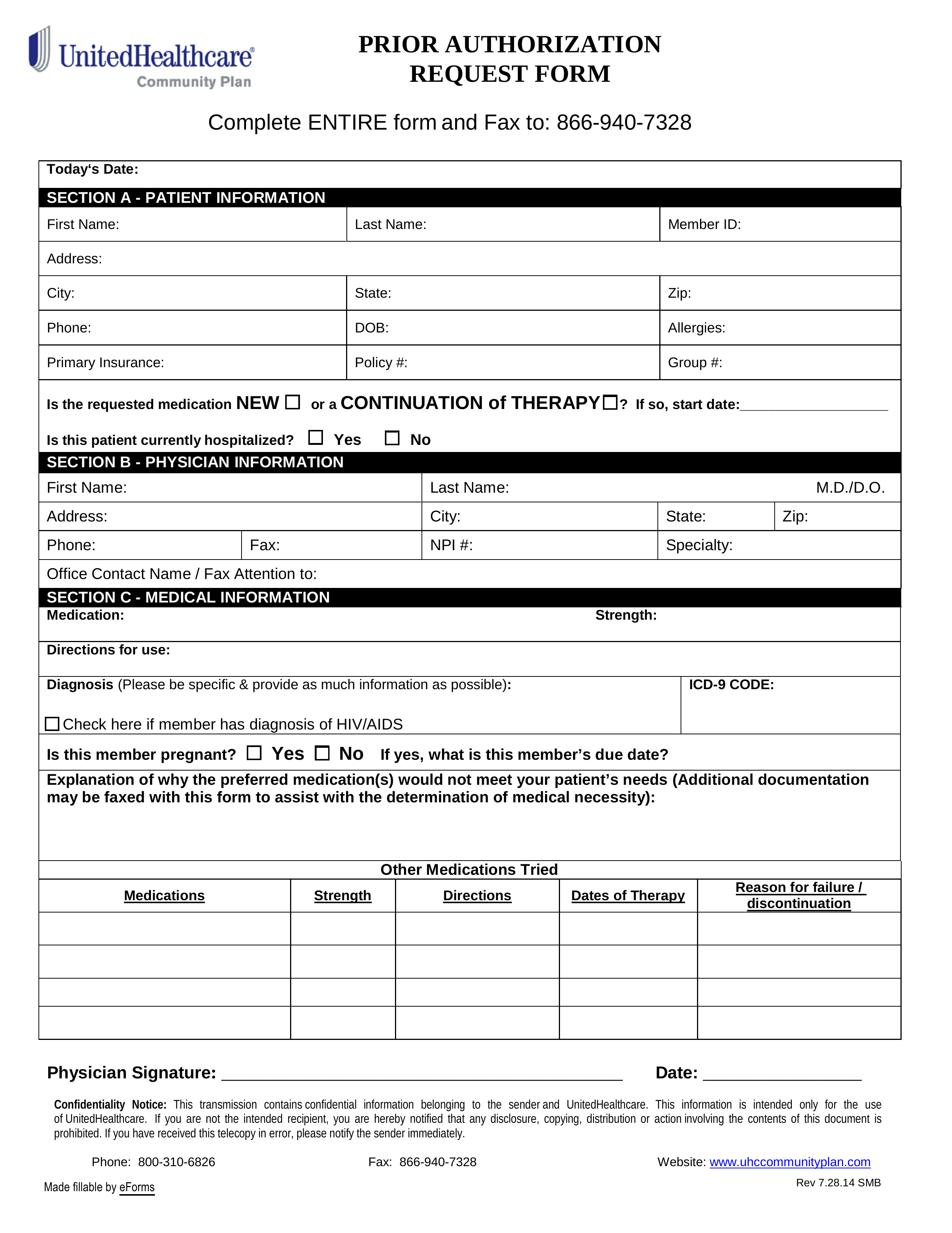
Free UnitedHealthcare Prior (Rx) Authorization Form PDF eForms
4) request a guarantee of payment; Web standardized prior authorization request form standardized prior authorization request form 3 this form does not replace payer specific prior authorization requirements. Web the standardized prior authorization form is intended to be used to submit prior authorization requests by fax. The form is designed to serve as a standardized prior authorization form accepted by.
It Is Intended To Assist Providers By Streamlining The Data Submission Process For Selected Services That.
4) request a guarantee of payment; Do not use this form to: Web electronically, through the issuer’s portal, to request prior authorization of a health care service. An attestation was added as a certification that any request submitted with the expedited timeframe meets the cms criteria.
☐ Initial Request Continuation/Renewal Request Reason For Request (Check All That Apply):
Web massachusetts standard form for medication prior authorization requests *some plans might not accept this form for medicare or medicaid requests. The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. Web the standardized prior authorization form is intended to be used to submit prior authorization requests by fax. Requesting providers should attach all pertinent medical documentation to support the request and submit to cca for review.
The New Form Is Now Available For Download On The Cca Website.
Web cca has a new standardized prior authorization form to ensure that minimal processing information is captured. Web what is the purpose of the form? Web ohio department of medicaid | 50 west town street, suite 400, columbus, ohio 43215. The prior authorization request form is for use with the following service types:
☐ Prior Authorization, Step Therapy, Formulary Exception
Web standardized prior authorization request form standardized prior authorization request form 3 this form does not replace payer specific prior authorization requirements. This form is being used for: